Achieving Stable Blood Glucose: A Practical Guide for Persons with Diabetes
13 Sep 2025```markdown
Achieving Stable Blood Glucose: A Practical Guide for Persons with Diabetes
Maintaining stable blood glucose levels is crucial for individuals with diabetes to prevent both short-term complications like hyperglycemia and hypoglycemia, as well as long-term issues such as nerve damage, kidney disease, and heart problems. This article serves as a comprehensive guide, providing practical strategies and insights to help you manage your blood sugar effectively. Diabetes Management For A Healthier Life Where To Start
Understanding Blood Glucose and Diabetes
Before diving into specific strategies, it's essential to understand what blood glucose is and how diabetes affects it. Blood glucose, also known as blood sugar, is the main sugar found in your blood and comes from the food you eat. Your body uses it for energy. Insulin, a hormone produced by the pancreas, helps glucose from food get into your cells to be used for energy. The 10 Minute Habit That Helps Stabilize Blood Sugar All Day Long
Diabetes occurs when your body doesn't make enough insulin (Type 1 diabetes) or can't effectively use the insulin it does produce (Type 2 diabetes). This leads to elevated blood glucose levels. Prediabetes occurs when blood glucose levels are higher than normal, but not high enough to be diagnosed as diabetes.
Key Strategies for Stable Blood Glucose
Here are practical strategies you can implement to help maintain stable blood glucose levels:
1. Nutrition Management
- Carbohydrate Counting: Learn how to count the grams of carbohydrates in your meals. Carbs have the most significant impact on blood glucose. Work with a registered dietitian or certified diabetes educator (CDE) to understand your individual carb targets.
- Portion Control: Pay attention to portion sizes. Using smaller plates can help with this.
- Choose Complex Carbohydrates: Opt for complex carbs like whole grains, fruits, vegetables, and legumes, which are digested more slowly than simple carbs (e.g., sugary drinks, white bread). This helps prevent rapid spikes in blood sugar.
- Include Fiber: High-fiber foods like vegetables, fruits, and whole grains help regulate blood glucose levels. Aim for 25-35 grams of fiber per day.
- Balanced Meals: Combine carbs with protein and healthy fats at each meal to slow down glucose absorption. For example, have whole-wheat toast with avocado and an egg instead of just toast.
- Limit Sugary Drinks: Avoid sugary drinks like soda, juice, and sweetened tea. These can cause rapid increases in blood glucose. Choose water, unsweetened tea, or diet soda instead.
2. Regular Physical Activity
- Consistency is Key: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, spread out over several days. Examples include brisk walking, cycling, and swimming.
- Strength Training: Incorporate strength training exercises at least twice a week. This helps improve insulin sensitivity.
- Check Blood Sugar Before and After Exercise: Monitor your blood sugar levels before, during, and after exercise, especially when starting a new activity. This helps you understand how your body responds to exercise and adjust your insulin or meal plan accordingly.
- Be Prepared: Carry a quick source of carbohydrates, such as glucose tablets or a small juice box, in case your blood sugar drops too low during exercise.
- Listen to Your Body: Pay attention to how you feel during exercise and adjust accordingly. If you experience dizziness, weakness, or other unusual symptoms, stop exercising and check your blood sugar.
3. Medication Management
- Follow Your Doctor's Instructions: Take your diabetes medications as prescribed by your doctor. Don't skip doses or change your dosage without consulting your healthcare provider.
- Understand Your Medications: Know the names, dosages, and potential side effects of all your medications.
- Monitor Blood Sugar Regularly: Regularly monitor your blood glucose levels as directed by your healthcare provider. This helps you track your progress and make necessary adjustments to your medication or meal plan.
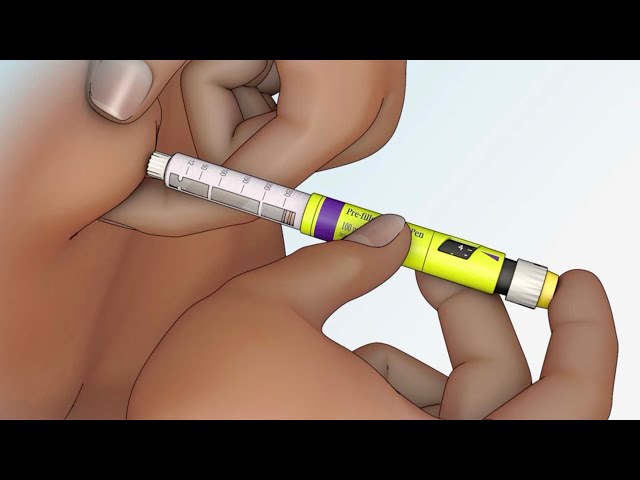
- Insulin Administration: If you use insulin, learn how to properly administer it and rotate injection sites to prevent skin problems.
4. Stress Management
- Practice Relaxation Techniques: Engage in relaxation techniques such as deep breathing exercises, meditation, or yoga to help manage stress.
- Get Enough Sleep: Aim for 7-8 hours of sleep per night. Lack of sleep can affect blood glucose levels.
- Engage in Hobbies: Participate in activities you enjoy to reduce stress and improve your overall well-being.
- Seek Support: Talk to a therapist or counselor if you're struggling to manage stress or cope with diabetes.
- Identify Stress Triggers: Understand what triggers your stress and develop coping mechanisms for those situations.
5. Regular Monitoring
- Blood Glucose Monitoring: Regularly check your blood glucose levels using a glucose meter or continuous glucose monitor (CGM) as advised by your healthcare provider.
- A1C Test: Get an A1C test at least twice a year to assess your average blood glucose levels over the past 2-3 months.
- Keep a Record: Maintain a log of your blood glucose readings, food intake, physical activity, and medications. This will help you identify patterns and make necessary adjustments to your management plan.
- Continuous Glucose Monitoring (CGM): Consider using a CGM system, which continuously monitors your blood glucose levels and provides real-time data. CGMs can help you identify trends and make informed decisions about your diabetes management.
6. Regular Doctor's Visits
- Routine Checkups: Schedule regular appointments with your doctor, CDE, and other healthcare professionals to monitor your health and make adjustments to your diabetes management plan.
- Eye Exams: Get an annual dilated eye exam to check for signs of diabetic retinopathy.
- Foot Exams: Get regular foot exams to check for nerve damage and other foot problems.
- Kidney Function Tests: Undergo regular kidney function tests to check for signs of diabetic nephropathy.
Troubleshooting Blood Glucose Fluctuations
Even with the best management efforts, you may still experience fluctuations in your blood glucose levels. Here are some common reasons for blood sugar fluctuations and how to address them: Surprising Factors Affecting Your Blood Sugar Control
| Reason | Solution |
|---|---|
| Overeating or consuming too many carbohydrates | Practice portion control and follow your carbohydrate targets. |
| Skipping meals or snacks | Eat meals and snacks on a regular schedule. |
| Inadequate insulin dosage (if on insulin) | Work with your doctor to adjust your insulin dosage. |
| Illness or infection | Monitor your blood glucose more frequently and follow your doctor's instructions. |
| Stress | Practice stress-reduction techniques. |
| Changes in physical activity level | Adjust your meal plan or medication as needed. |
| Dawn phenomenon (early morning blood glucose increase) | Discuss with your doctor if medication adjustments are needed. |
Emergency Situations: Hypoglycemia and Hyperglycemia
Knowing how to handle emergency situations like hypoglycemia (low blood glucose) and hyperglycemia (high blood glucose) is essential for people with diabetes.
- Hypoglycemia: Defined as blood glucose below 70 mg/dL. Symptoms include shakiness, sweating, dizziness, hunger, confusion, and irritability. Treat it by consuming 15-20 grams of quick-acting carbohydrates (e.g., glucose tablets, juice). Recheck blood sugar after 15 minutes and repeat treatment if necessary. If the person is unconscious, administer glucagon and call for emergency medical assistance.
- Hyperglycemia: Defined as blood glucose above your target range. Symptoms include frequent urination, excessive thirst, blurred vision, and fatigue. Take steps to lower your blood glucose, such as drinking water, exercising (if appropriate), and adjusting your medication (as directed by your doctor). If blood glucose remains high or you experience symptoms of diabetic ketoacidosis (DKA) such as nausea, vomiting, abdominal pain, and fruity-smelling breath, seek immediate medical attention.
The Role of Support Systems
Managing diabetes can be challenging, so building a strong support system is crucial. This may include:
- Family and friends: Educate your loved ones about your diabetes and how they can support you.
- Support groups: Join a diabetes support group to connect with others who understand your challenges.
- Healthcare professionals: Work closely with your doctor, CDE, and other healthcare professionals to develop and implement a comprehensive management plan.
Conclusion
Achieving stable blood glucose levels requires a combination of strategies, including nutrition management, regular physical activity, medication management, stress reduction, and regular monitoring. By implementing these strategies and working closely with your healthcare team, you can effectively manage your diabetes and reduce your risk of complications. Remember, consistency and self-awareness are key to success. This practical guide provides the foundation for a healthier, more balanced life with diabetes. ```
By Gregory W. Barsness, M.D.
